Below Deck’s Aesha Scott Joins Leah Shafer and Top Doc for Real Talk About Breast Cancer [Exclusive]
Facing a possible breast cancer diagnosis is scary, but catching it early can be lifesaving. For Captain Sandy Yawn‘s girlfriend, Leah Shafer, early detection made all the difference.
Shafer has LCIS (atypical lobular carcinoma in situ), which is “a condition where abnormal cells are found in the lobules of the breast. It is considered a non-invasive form of breast cancer, but it does increase the risk of developing invasive breast cancer in the future,” Shafer shared on Instagram.
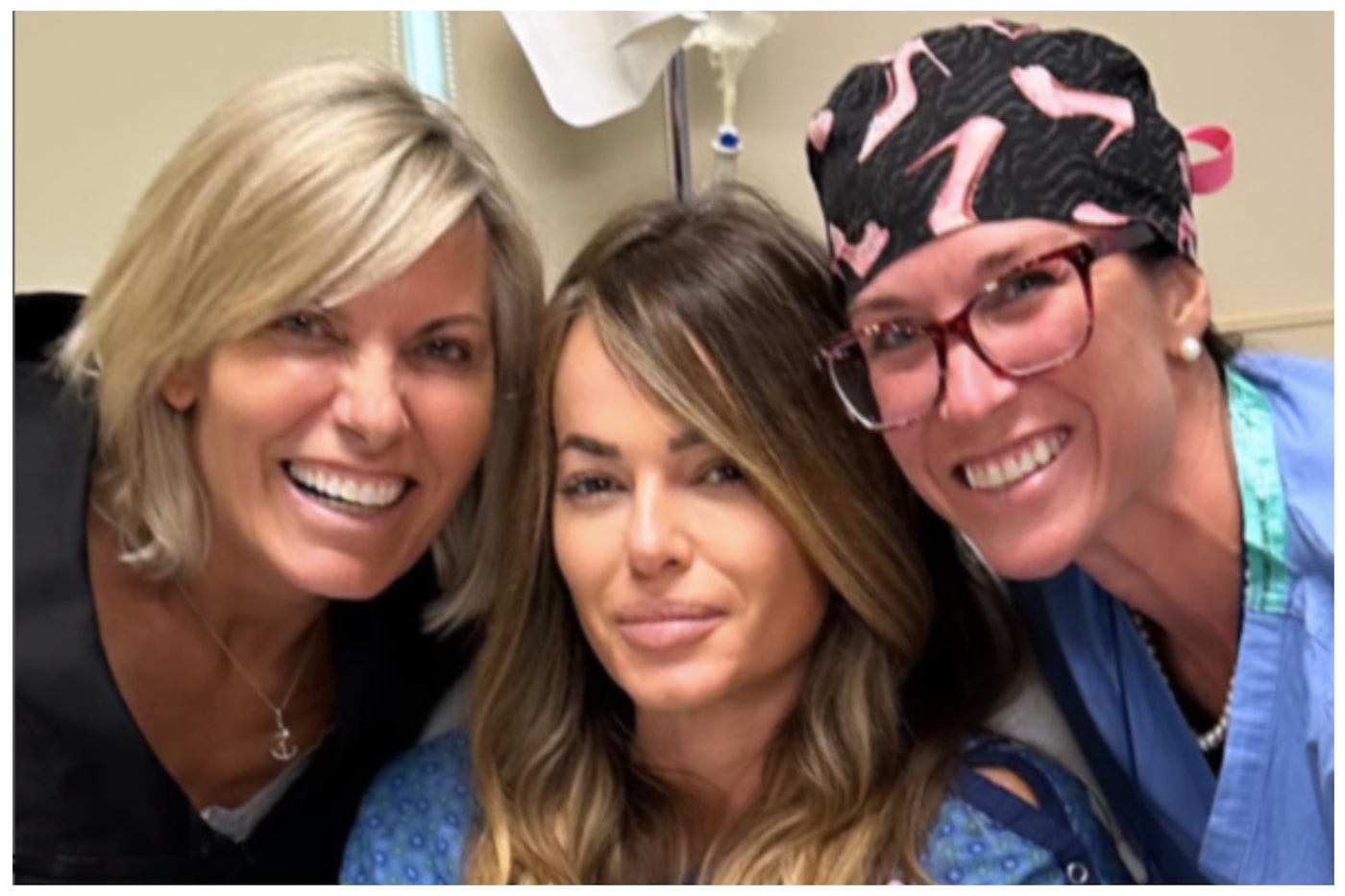
She gets checked every six months and recently had a biopsy and her second lumpectomy. Shafer turned to breast surgical oncologist, Dr. Kayla Griffith for her surgery – who happens to be a close friend of Below Deck Down Under‘s chief stew Aesha Scott.
“When I first moved to Breckenridge, because as a lot of people know, my partner, he is Kiwi but he’s got dual citizenship,” Scott explained. “And so when we got together, maybe like three and a half years ago now, when I found out it was getting serious, I was like, I need to make friends in the area. I don’t want to be that girl that’s always with a boyfriend. And so I quickly made a group of friends and Kayla was one of the people in this group of friends. And now she’s not able to get rid of me.”
The conincidence was kismet. So Shafer, Scott, and Griffith wanted to use their platforms to raise awareness and let people know that early detection saves lives. The powerhouse trio hopped on an Instagram Live, alongside Showbiz Cheat Sheet to start a conversation.
Leah Shafer discovered her breast cancer risk during a routine screening
Griffith acknowledged that most women put themselves last when it comes to their health. “We all get so busy taking care of everybody else that we really put ourselves on the back burner and we don’t do the things that we need to do because somebody’s got to get to soccer practice,” she said. “But if you take the time and put yourself first it actually helps you and your family.”
“So you catch things early, just like Leah your recent scare that I know you’ve been pretty open about,” she continued. “But when you can catch high-risk lesions early or even a breast cancer early, something is very treatable at a stage 1 breast cancer versus of stage 3 and 4,” which is when chemotherapy could be involved.
Shafer only learned about her condition during a routine screening. “Two years ago I went in for my screenings because my grandmother had breast cancer,” she recalled. “So I’m very proactive. And I just wanted to make sure I was OK. But I found out that I had a rare disorder called LCIS so I have a higher risk of getting breast cancer. And so I had a lumpectomy two years ago and then it showed up again on the other side.”
Griffith said the LCIS diagnosis carries a high-risk cancer development in both breasts.
Aesha Scott wondered if she should start getting mammograms
Scott, who is 31 years old wondered if she should be getting mammograms at her age. “There’s a one in eight risk of developing breast cancer,” Griffith explained. “So the age that we generally start mammograms is 40. But, if you have more of a high-risk family history, your mom, your sister, your aunt. If your dad had breast cancer. Any male breast cancer in the family or family histories of pancreatic cancer … we do genetic testing. But also, if you just have a risk and don’t have a genetic mutation, we scootch up that age.”
“But at 31, you should be feeling those girls!” Griffith laughed. referring to breast self exams.
“One of my grandmothers, had breast cancer, so does that count as being at higher risk?” Scott asked.
“It definitely adds to your risk,” Griffith said. “There’s an algorithm we use of family history. How young were you at your first period? Have you had a child? We start adding in the family history as well. But yeah, having a grandmother with breast cancer, especially if she was under the age of 50.”
“Now we are kind of advocating for getting genetic testing on people because you may carry a genetic mutation you don’t know about. If you’re not going in to get it checked out you wouldn’t know that,” Griffith said.
What are mammograms and biopsies really like?
Griffith advocates for partnering an ultrasound with a mammogram for patients with dense breast tissue. Also, being checked every six months, instead of yearly can catch early breast cancers in higher-risk patients.
Plus, gone are the days of painful mammograms. “I remember my mom complaining growing up that she finds it really painful because she’s got little bittie titties. So they kind of have to really squeeze them to get a good reading,” Scott said.
“We’ve come a long way with the mammogram,” Griffith said. “We still say they are created by a man [laughed].”
But what about getting a biopsy? “Honestly, it was painless. They numbed me. So I didn’t feel a thing. They just took a little tissue and that was it,” Shafer recalled, adding that waiting for the results was the hardest part. “But it’s an ultrasound and guided biopsy so everything is very precise.”
Dr. Griffith discusses exciting new breast cancer mastectomy reconstruction approach
Learning that she didn’t have cancer gave Shafer significant peace of mind. However, if this happens yet again, she may go for a full mastectomy, which has come a very long way in the past few years.

“We specialize in nipple-sparing mastectomy, and we can actually make that look great. It doesn’t have to be stigmatizing and cosmetically disfiguring,” Griffith said. “I work in tandem with plastic surgeons. I start on one side, remove the breast tissue, saving the skin, and the nipple envelope and will move to the other side. Plastic surgeon tags in. We are in open to close is one single surgery directly to implant and in 3 1/2 to 4 hours, you go home that day.”
For more information about Dr. Griffith and her specialisties visit here.
Griffith, Scott, and Shafer hoped that the Instagram Live ultimately helped to save lives. Plus, Shafer and Griffith said they are open to any follow-up questions that can be sent directly on Instagram.



